
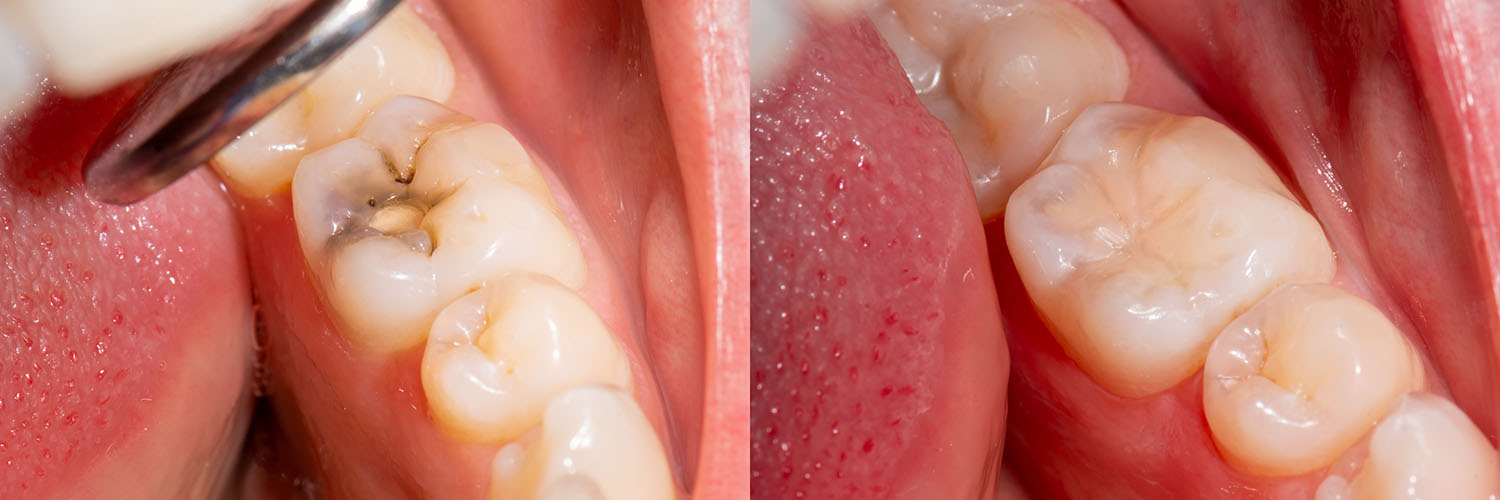
When a cavity or minor fracture weakens a tooth, a carefully placed filling restores its strength and helps prevent further damage. Addressing decay early preserves more of your natural tooth and reduces the chance that a small problem will require a larger restoration later on.
Tooth decay remains common across all age groups, so placing fillings is one of the most frequently performed restorative procedures in dental care. Because it is so routine, modern dentistry focuses on techniques and materials that prioritize durability, comfort, and a natural appearance.
The office of Premier Dentistry takes a conservative, evidence-based approach to restorations: our goal is to remove only the damaged tissue and rebuild the tooth so it looks, feels, and functions as closely to the original as possible. We couple modern materials with precise techniques to deliver reliable results for patients of all ages.
People have attempted to restore damaged teeth for millennia. Archaeological finds show rudimentary dental repairs dating back thousands of years, while the 19th and 20th centuries brought widespread use of metal-based restorations such as gold and amalgam.
Over the last several decades, material science and adhesive dentistry have transformed how we rebuild teeth. New composite resins, glass ionomers, ceramics, and other options allow clinicians to offer restorations that are both strong and more visually discreet than traditional metal fillings.
Restorative treatment begins with a careful assessment: we evaluate the extent of decay, the remaining tooth structure, and how the tooth interacts with adjacent teeth when you bite and chew. That evaluation informs our choice of material and technique so your restoration performs well under everyday use.
Wherever possible, we preserve tooth structure and use adhesive methods that reinforce the remaining enamel and dentin. That philosophy helps prolong the life of the restoration while maintaining the tooth’s natural contours and appearance.
Communication is an important part of the process. We’ll explain the recommended options, the steps involved, and what you can expect at each appointment so you can make an informed decision about your care.

Today’s restorative options go beyond simple function — many are designed to match the color and translucency of natural teeth while providing excellent wear resistance. The right choice depends on the tooth’s location, the size of the cavity, aesthetic preferences, and the long-term goal for the restoration.
Some materials bond directly to the tooth, helping to seal the interface and reduce the risk of leakage. Others are fabricated outside the mouth and cemented in place to repair larger defects while preserving the remaining healthy tooth structure.
Composite fillings are a blend of resin and finely ground glass or ceramic particles. They are available in a range of shades so a trained clinician can match the restoration to your tooth, producing a discreet result that blends with your smile.
Because composites bond to the tooth, they can help reinforce weakened structure and often require less removal of healthy tissue during placement. They are an excellent choice for visible front teeth as well as smaller restorations in the back of the mouth. With proper care, composites provide a durable and attractive restoration for many years.
Amalgam has a long history of use because of its strength and wear resistance, especially in high-stress chewing areas. While not tooth-colored, amalgam remains a practical option for certain posterior restorations where durability is the primary concern.
Placement is straightforward and reliable, and for larger cavities in back teeth it can still be an effective restorative material when a cosmetically matched solution is not required.
Glass ionomer materials bond chemically to tooth structure and release fluoride over time, which can offer extra protection against recurrent decay. They are often used in areas where moisture control is difficult, for small restorations near the gumline, or in primary (baby) teeth.
While glass ionomers are convenient and tooth-friendly, they are less wear-resistant than other options and are typically used where strength requirements are lower or as a temporary measure during multi-step care.
Ceramic restorations are crafted from high-strength dental porcelain and are fabricated in a lab or dental milling center. Because they are made outside the mouth, they can provide a precise fit and outstanding aesthetics for larger areas of damage.
Inlays and onlays preserve more natural tooth structure than full crowns and are an excellent restorative choice when a direct filling would be insufficient to restore form and function over the long term.
Gold remains a reliable, long-lasting restorative material with excellent wear characteristics and biocompatibility. Although less commonly selected today for aesthetic reasons, gold restorations perform exceptionally well in demanding biting environments and can last for many decades when cared for properly.
The repair process begins with an exam that may include visual inspection, dental X-rays, and careful evaluation of your bite. These tools help determine how extensive the decay is and whether a simple filling or a more protective restoration is needed.
Once treatment is planned, the affected area is numbed with local anesthesia so the procedure is comfortable. The clinician removes the decayed tissue using precision instruments — this can include traditional rotary instruments, air abrasion, or other minimally invasive tools depending on the situation and patient preference.
After the cavity is prepared, the selected material is placed and shaped to restore the tooth’s anatomy. Composites are layered and cured with a specialized light, while glass ionomers are placed and allowed to set. Indirect restorations such as inlays or onlays are fabricated off-site and bonded into place on a subsequent visit.
For patients who have dental anxiety, our team can discuss gentle options and appropriate sedation approaches so you remain relaxed and comfortable throughout care.
Recovery from a filling is usually quick. Numbness from anesthesia typically wears off within a couple of hours, and most people return to normal activity the same day. There are a few things to keep in mind as your tooth adjusts to the restoration.
Protect yourself while numb
After your appointment, avoid chewing until the anesthesia has fully worn off to prevent accidental biting of the cheek, lip, or tongue. Hot foods and beverages should also be approached cautiously until sensation returns.
Expect a short period of adjustment
Your tooth may feel slightly different initially as you become accustomed to the restoration. If your bite feels uneven or you notice persistent discomfort, contact our office for a quick adjustment.
Temporary sensitivity is common
Sensitivity to hot, cold, or pressure can occur after a filling but usually subsides within days to a few weeks. If sensitivity increases or is accompanied by sharp, lingering pain, schedule an evaluation to rule out other issues.
Long-term care helps protect your restoration
Routine oral hygiene, including brushing with fluoride toothpaste, daily flossing, and regular dental checkups, helps extend the life of any restoration. During exams, we monitor fillings for wear and address concerns early to prevent larger problems.
We encourage patients to ask questions before and after treatment so they feel confident in their care. If you notice anything unusual following your appointment, reach out and we will advise you on the appropriate next steps.

Fillings are a long-term solution, but like any dental work they require attention. Regular professional exams and cleanings let your dental team monitor restorations for small signs of wear or breakdown before they become larger problems.
Simple preventive habits — consistent brushing, flossing, limiting frequent sugary snacks, and using fluoride products as recommended — reduce the risk of new decay and protect both natural teeth and existing restorations.
If you have concerns about an older filling or notice changes in your bite or sensitivity, bring it to our attention. Early intervention often allows for conservative repairs and better long-term outcomes.
In summary, modern dental fillings offer effective ways to restore teeth with an emphasis on preserving tooth structure, maintaining function, and achieving an aesthetic result. If you’d like to learn more about restorative options or how Premier Dentistry approaches fillings and preventive care, please contact us for more information.
Dental fillings are restorations used to repair teeth damaged by decay or small fractures. They restore a tooth's strength and shape so it can function normally for chewing and speaking. Fillings also seal the affected area to protect against further decay.
Fillings are indicated when decay has not progressed to the point of needing a crown or root canal therapy and when enough healthy tooth structure remains to support a restoration. Early detection and treatment allow for more conservative repairs that preserve natural tooth tissue. Your clinician will recommend the appropriate type of filling based on the extent of damage and your oral health goals.
Several modern materials are used for fillings, each with different properties and advantages. Composite resins are tooth-colored and bond to enamel and dentin, allowing conservative preparations. Amalgam is a durable metal alloy traditionally used in high-stress areas, while glass ionomer releases fluoride and bonds chemically to tooth structure.
For larger defects, indirect options such as porcelain or ceramic inlays and onlays are fabricated outside the mouth and bonded into place to restore form and function. Gold remains an excellent long-term option for posterior teeth where appearance is less important. Your clinician will weigh factors like location, size, aesthetics, and longevity when recommending a material.
Treatment begins with a comprehensive exam that may include visual inspection and dental X-rays to assess the extent of decay and the health of surrounding tissues. Local anesthesia is used to numb the area so the procedure is comfortable, and sedation options can be discussed for anxious patients. The dentist removes decayed tissue using precise instruments while preserving as much healthy structure as possible.
Once the cavity is prepared, the chosen material is placed and finished to restore proper anatomy and bite; composite fillings are layered and cured with a light, while glass ionomers set chemically and indirect restorations are bonded on a subsequent visit. The bite is checked and adjusted to ensure comfortable function, and the team will review aftercare instructions before you leave. At Premier Dentistry we focus on conservative techniques and clear communication so patients understand their options and recovery expectations.
During the appointment most patients feel little to no pain because local anesthesia numbs the treated tooth and surrounding tissues. If dental anxiety is a factor, the team can discuss nitrous oxide or other calming measures to help you remain relaxed. Modern techniques and steady communication help make the experience comfortable for children and adults alike.
It is normal to experience some sensitivity to hot, cold, or pressure for a few days to weeks after a filling as the tooth adjusts to the restoration. If you notice sharp, lingering pain, swelling, or if the sensitivity worsens instead of improving, contact the office for an evaluation to rule out underlying issues. A simple bite adjustment or additional treatment often resolves most post-operative concerns.
The lifespan of a filling depends on the material used, the size and location of the restoration, and the forces placed on the tooth during chewing. Composite fillings typically provide many years of service in properly maintained mouths, while amalgam and high-quality indirect restorations such as ceramics or gold can last longer under heavy wear. Regular monitoring helps determine when a repair or replacement is needed.
Factors that influence longevity include oral hygiene, diet, bruxism (tooth grinding), and the quality of the initial restoration. Routine dental exams and professional cleanings let the dentist detect early wear, marginal breakdown, or recurrent decay before problems progress. When detected early, repairs are often conservative and preserve more natural tooth structure.
When a cavity is very large, involves a cusp, or the remaining tooth structure is insufficient to support a direct filling, the dentist may recommend an inlay, onlay, or full crown. Inlays and onlays are partial restorations that preserve more of the tooth than a crown while providing enhanced strength for larger defects. Crowns encase the entire visible tooth and are preferred when extensive restoration is necessary to protect long-term function.
The choice between these options depends on how much healthy tooth remains, the location of the tooth, and functional demands such as chewing forces. Indirect restorations are fabricated from strong, tooth-colored ceramics or metal alloys and are bonded or cemented into place for durability. Your clinician will review the benefits and steps involved so you can make an informed decision.
Advances in adhesive dentistry and composite materials have significantly improved the strength and wear resistance of tooth-colored fillings. Composites bond to the tooth and can help reinforce weakened structure, which is beneficial for many restorations. In some high-stress posterior situations, metal restorations may still offer superior longevity.
The optimal material is selected based on the individual clinical scenario rather than a one-size-fits-all answer; considerations include the size of the cavity, occlusion, aesthetics, and patient preferences. A dentist evaluates these factors and explains the trade-offs so patients understand performance expectations. Proper placement and oral care are essential to maximizing the life of any restoration.
Cavity diagnosis begins with a thorough clinical exam and may include bitewing or periapical X-rays to visualize interproximal decay and assess the depth of lesions. Additional tools such as intraoral cameras, transillumination, or diagnostic probes can provide further information about early enamel lesions. The clinician also evaluates the tooth's role in the bite to determine how restoration will affect overall function.
After a complete assessment the dentist recommends the least invasive effective treatment, which may range from preventive measures and monitoring to a direct filling or a larger indirect restoration. The treatment plan considers the patient's oral health history, risk of recurrent decay, and restorative goals. Clear communication about options and expected outcomes helps patients participate in decision-making.
Certain materials, notably glass ionomer cements, release fluoride over time which can provide a modest protective effect against recurrent decay at the margin of the restoration. Bonded restorations such as composites and glass ionomers also help seal the interface between tooth and filling, reducing pathways for bacteria. These material properties can contribute to overall oral health but do not replace good hygiene and preventive care.
Preventing future decay relies primarily on consistent brushing with fluoride toothpaste, daily flossing, limiting frequent sugary snacks, and regular professional exams and cleanings. Sealants, topical fluoride treatments, and individualized preventive plans are additional tools your dentist may recommend based on risk. Routine monitoring ensures restorations remain intact and healthy so early problems can be addressed conservatively.
After a filling expect numbness for a few hours, so avoid chewing until sensation returns and take care with hot foods or beverages to prevent accidental injury. Maintain normal oral hygiene, being gentle around the treated tooth at first, and resume regular brushing and flossing as comfort allows. Minor soreness or sensitivity is common and typically improves within days to weeks.
Contact the office promptly if you experience persistent sharp pain, swelling, prolonged numbness, a filling that feels high when you bite, or if the restoration fractures or falls out. These signs can indicate the need for a quick adjustment or further evaluation to prevent complications. Premier Dentistry can arrange follow-up care and provide guidance to restore comfort and function.
